Latest
Articles
Browse our recent articles by MSK Direct
Not All PRP Is the Same — Why the Details Matter When Pain Hasn’t Improved
If you’ve been dealing with persistent tendon or joint pain—and physical therapy, medications, or standard injections haven’t helped—it’s natural to look toward PRP (platelet-rich plasma) as the next step. PRP is often described as “using your body to heal itself.”
That idea is true. But here’s the part many patients never hear:
Not all PRP is the same.
And those differences can meaningfully affect comfort, recovery, and results.
The Core Problem: PRP Isn’t a Single Product
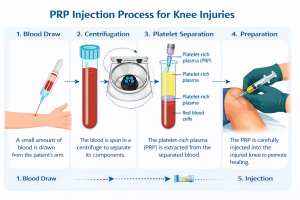
PRP isn’t a factory-made drug with a fixed dose. It’s a biologic made from your blood at the time of treatment. The kit used to process that blood determines what actually gets injected.
Think of it like coffee. An espresso and a watered-down americano both start with coffee beans—but they deliver very different experiences.
What Actually Makes PRP Different?
 1. How Many Platelets You Receive (The “Dose”)
1. How Many Platelets You Receive (The “Dose”)
The most important variable is platelet dose—the total number of platelets delivered, not just how “concentrated” they sound on marketing materials.
- For large joints like the knee, research suggests a therapeutic target around 10 billion platelets
- Some systems struggle to reach that threshold in a single treatment
- Higher-efficiency systems can get closer in one session, reducing the need for repeat injections
A “5× concentration” sounds impressive—but if the volume is small, the total dose may still fall short.
2. Cellular Purity: What’s Mixed In
PRP isn’t just platelets—it can also contain red and white blood cells.
- Red blood cells (RBCs): Too many can increase inflammation and post-injection pain
- White blood cells (WBCs):
- Helpful in some tendon problems
- Often not ideal for arthritic joints, where excess inflammation can worsen symptoms
Advanced systems allow clinicians to adjust this balance based on whether the problem is a tendon or a joint. Simpler kits don’t offer that control.
3. Safety: Closed vs. Open Systems
How PRP is prepared matters for sterility.
- Closed systems keep the blood sealed from the environment throughout processing
- Open systems expose the sample to room air, which increases contamination risk—especially outside of surgical-grade environments
This difference rarely gets discussed, but it’s foundational to patient safety.
4. Processing Method
Some kits use:
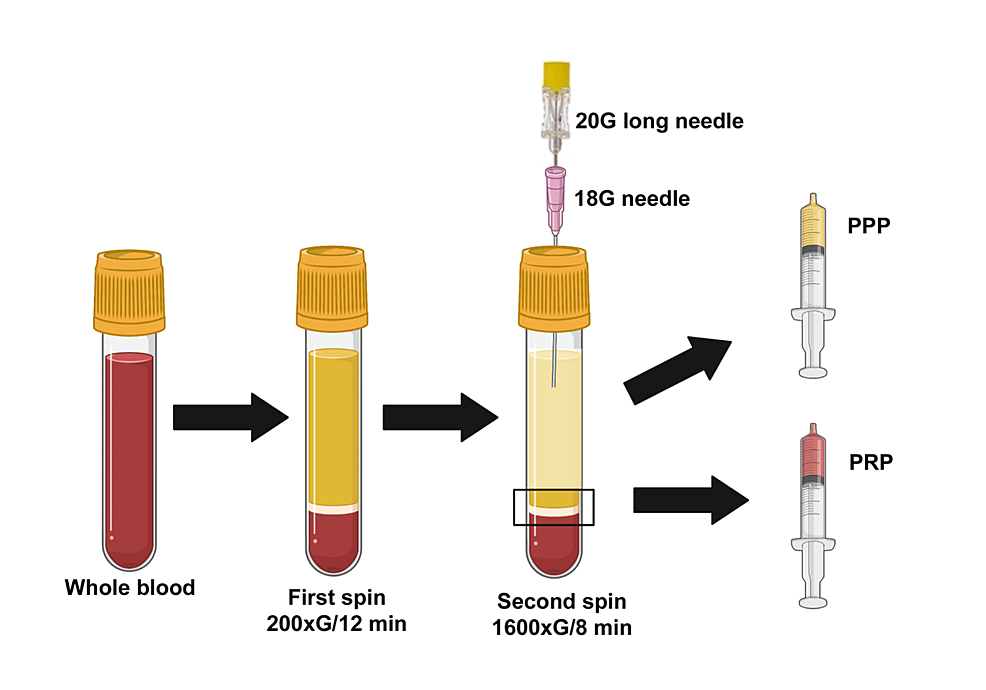
- Single-spin centrifugation (simpler, often lower yield)
- Double-spin protocols (more steps, higher platelet recovery)
The method changes how many platelets are captured—and how consistent the final product is.
5. True Cost vs. Sticker Price
A cheaper kit upfront can end up costing more if:
- Platelet dose is low
- Multiple injections are required to reach a therapeutic effect
A useful way to think about value is “cost per billion platelets,” not cost per injection.
Why This Matters for You
If PRP didn’t help someone you know—or didn’t help you in the past—it doesn’t necessarily mean PRP “doesn’t work.” It may mean the biologic dose or formulation wasn’t right for the tissue being treated.
PRP isn’t one treatment. It’s a category of treatments.
The Takeaway
PRP works by delivering a biologic signal to damaged tissue—but:
- Dose matters
- Purity matters
- Customization matters
- Safety matters
When those pieces are aligned, PRP can be a powerful option for stubborn tendon and joint pain that hasn’t responded to conservative care.
Curious if PRP Could Still Be an Option for You?
If you’re dealing with ongoing pain and want clarity on whether PRP—and which type—makes sense for your situation, a focused consultation can help map out next steps.
Understanding the details is often the difference between “I tried PRP” and “PRP actually helped.”



Leave a Reply